This pulmonary embolism NCLEX review is a free resource to enhance your understanding of this medical condition.
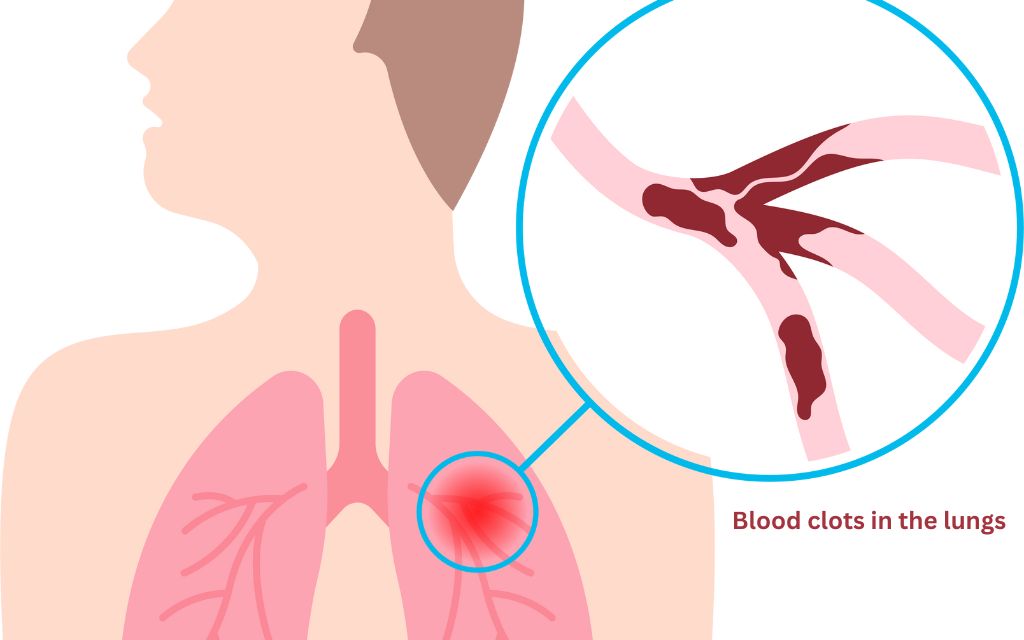
Pulmonary embolism (PE) is a serious medical condition that occurs when a blood clot blocks one of the pulmonary arteries in the lungs. This can cause chest pain, breathlessness, and cough.
Quick facts!
- PE is caused by a blood clot blocking an artery in the lung.
- Blood clots most often start in the legs and travel up through the right side of the heart and into the lungs.
- There are several risk factors for developing PE.
- Symptoms can vary depending on the size and location of the clot.
- Diagnosis is based on medical history, physical exam, and test results.
- Treatment focuses on preventing existing clots from getting bigger and preventing new clots from forming.
- PE can be life-threatening if not diagnosed and treated promptly.
- Prevention measures such as wearing compression stockings, staying hydrated, and avoiding prolonged periods of immobility can reduce the risk of developing PE.
What is a pulmonary embolism?
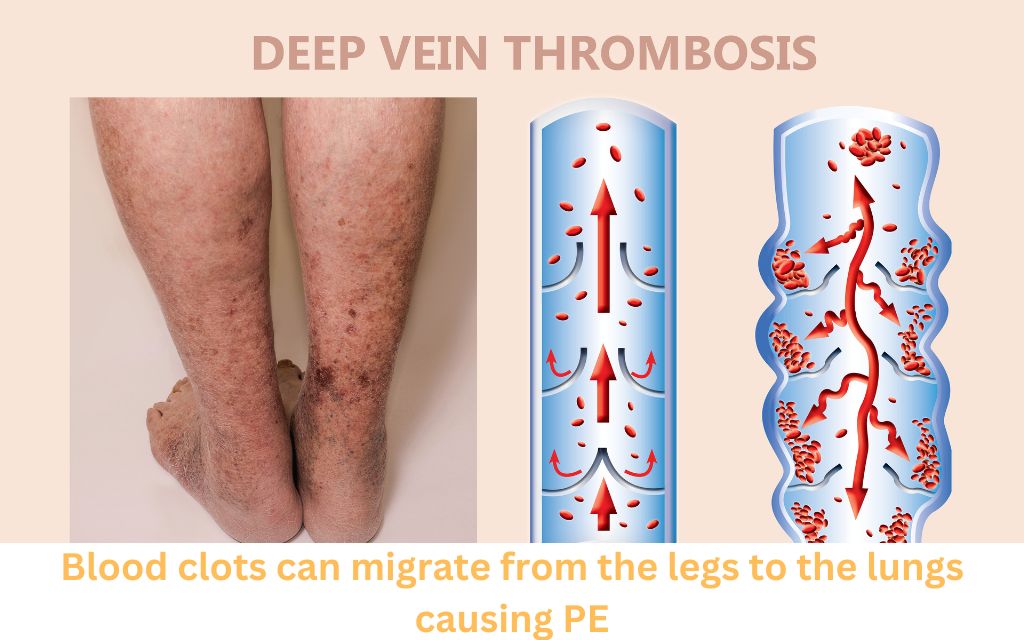
A pulmonary embolism occurs when a blood clot gets stuck in an artery in the lung, blocking blood flow to part of the lung.
Blood clots most often start in the legs and travel up through the right side of the heart and into the lungs.
This is called deep vein thrombosis (DVT).
Risk factors for developing pulmonary embolism
- Deep vein thrombosis (DVT)
- Alterations in normal blood flow (stasis) or prolonged immobilization
- Pregnancy
- Surgery
- Medications such as birth control pills or estrogen
- Polycythemia (an increase in red blood cells in the body)
- Cancer
- Family history
- Damage to walls of blood vessels
Signs and symptoms of pulmonary embolism
The signs and symptoms of PE can vary depending on the size and location of the clot. Some common symptoms include:
- Sudden onset of shortness of breath
- A feeling of impending doom
- Anxiety and restlessness
- Petechial rash over the chest and axillae – pinpoint, round spots that appear as a result of bleeding
- Low oxygen saturation levels
- Coughing up blood
- Rapid heartbeat and breathing
- Lightheadedness or fainting
Types of pulmonary embolism
There are two main types of PE: acute and chronic.
Acute pulmonary embolism occurs suddenly and can be life-threatening.
A chronic pulmonary embolism develops over time and can lead to long-term complications such as pulmonary hypertension.
Diagnostics/testing
Diagnosing PE can be challenging because its symptoms overlap with those of other conditions.
Diagnosis is based on careful consideration of medical history, physical exam, and test results, including those that help rule out other conditions.
Some tests that may be used to diagnose PE include:
- Electrocardiogram (ECG or EKG)
- CT pulmonary angiogram
- X-ray
- Spiral CT
- Ventilation-perfusion scan
- D-dimer test
Nursing interventions for pulmonary embolism
Nursing interventions for a patient with pulmonary embolism includes a variety of interventions aimed at managing the condition and preventing complications.
Some of the key nursing interventions for patients with pulmonary embolism include:
- Encourage ambulation and active and passive leg exercises to prevent venous stasis.
- Monitor thrombolytic therapy: INR (International Normalized Ratio) or PTT (Prothrombin Time Test)
- Pain Management: Administer pain medication as prescribed and use non-pharmacological methods such as positioning and relaxation techniques to manage pain.
- Anxiety Management: Provide emotional support and reassurance to help relieve anxiety. Educate the patient about their condition and treatment plan to help reduce fear and uncertainty.
- Oxygen therapy: Administer oxygen therapy as prescribed to maintain oxygen levels in the arterial blood.
- Prevent the formation of a thrombus: Encourage ambulation, active and passive leg exercises, and the use of compression stockings to prevent the formation of a thrombus.
- Monitor vital signs and oxygen saturation levels: Regular monitoring is required to assess the patient’s condition and response to treatment.
- Assist with mobility: Assist the patient with mobility and encourage physical activity as tolerated.
- Educate patients on prevention measures such as wearing compression stockings, staying hydrated, and avoiding prolonged periods of immobility.
These are some of the key nursing interventions for patients with PE.
It is important for nurses to closely monitor the patient’s condition, administer medications as prescribed, provide emotional support, and educate the patient on prevention measures to help manage the condition and prevent complications.
Priority nursing actions for suspected pulmonary embolism
- Obtain vital signs and check lung sounds
- Notify the health care provider
- Reassure the client and elevate the head of bed
- Prepare to administer oxygen
- Prepare to obtain an arterial blood gas
- Prepare to administer heparin
Treatment for pulmonary embolism- pharmacological and non-pharmacological
Treatment for PE focuses on preventing existing clots from getting bigger and preventing the formation of new clots.
Non-pharmacological treatments may include: WES
- Wearing compression stockings
- Elevating the legs
- Staying active
Anticoagulant
The main( pharmacological)treatment for pulmonary embolism is called an anticoagulant.
This is a drug that causes chemical changes in your blood to stop it from clotting easily.
They include HWF
- Heparin,
- Warfarin,
- Fondaparinux
Thrombolytic medications
Thrombolytic medications may be used to dissolve existing clots. They include
- Anistreplase
- Streptokinase
- Urokinase
In some cases, surgical embolectomy may be necessary to remove a large or life-threatening clot.
Mnemonics
- ATI is the treatment of PE. A stands for Anticoagulant. T stands for Thrombolytic medications and I stand for Interventional therapies
- HWF Helps Prevent Pulmonary Emboli: H stands for Heparin. W stands for Warfarin and F stands for Fondaparinux
I hope you found this NCLEX review helpful. Share this post!
Check out my blog post on COPD here!
Sources
Pulmonary embolism – Mayo Clinic https://www.mayoclinic.org/diseases-conditions/pulmonary-embolism/symptoms-causes/syc-20354647
What is Pulmonary Embolism – John Hopkins University https://www.hopkinsmedicine.org/health/conditions-and-diseases/pulmonary-embolism
How serious is Pulmonary Embolism – Cleveland Clinic https://my.clevelandclinic.org/health/diseases/17400-pulmonary-embolism
