What is Diabetes Ketoacidosis?
It’s a life-threatening issue that occurs when the body cannot produce sufficient insulin to meet its demands. Insulin helps convert glucose into energy for the body’s cells.
Diabetes ketoacidosis, also known as DKA, affects Type 1 diabetes patients and is caused by insufficient insulin and illness.
Patients with Type 1 diabetes cannot produce insulin and require insulin therapy for the rest of their lives.
When there’s a low level or no insulin in the blood to convert glucose to be stored in the body cells for energy, fats are broken down as a compensatory mechanism to provide energy for the body, and this results in the production of ketone bodies.
It causes a buildup of ketones in the blood and, if left untreated, can lead to ketoacidosis. What are the main symptoms to observe if someone has this disease condition?
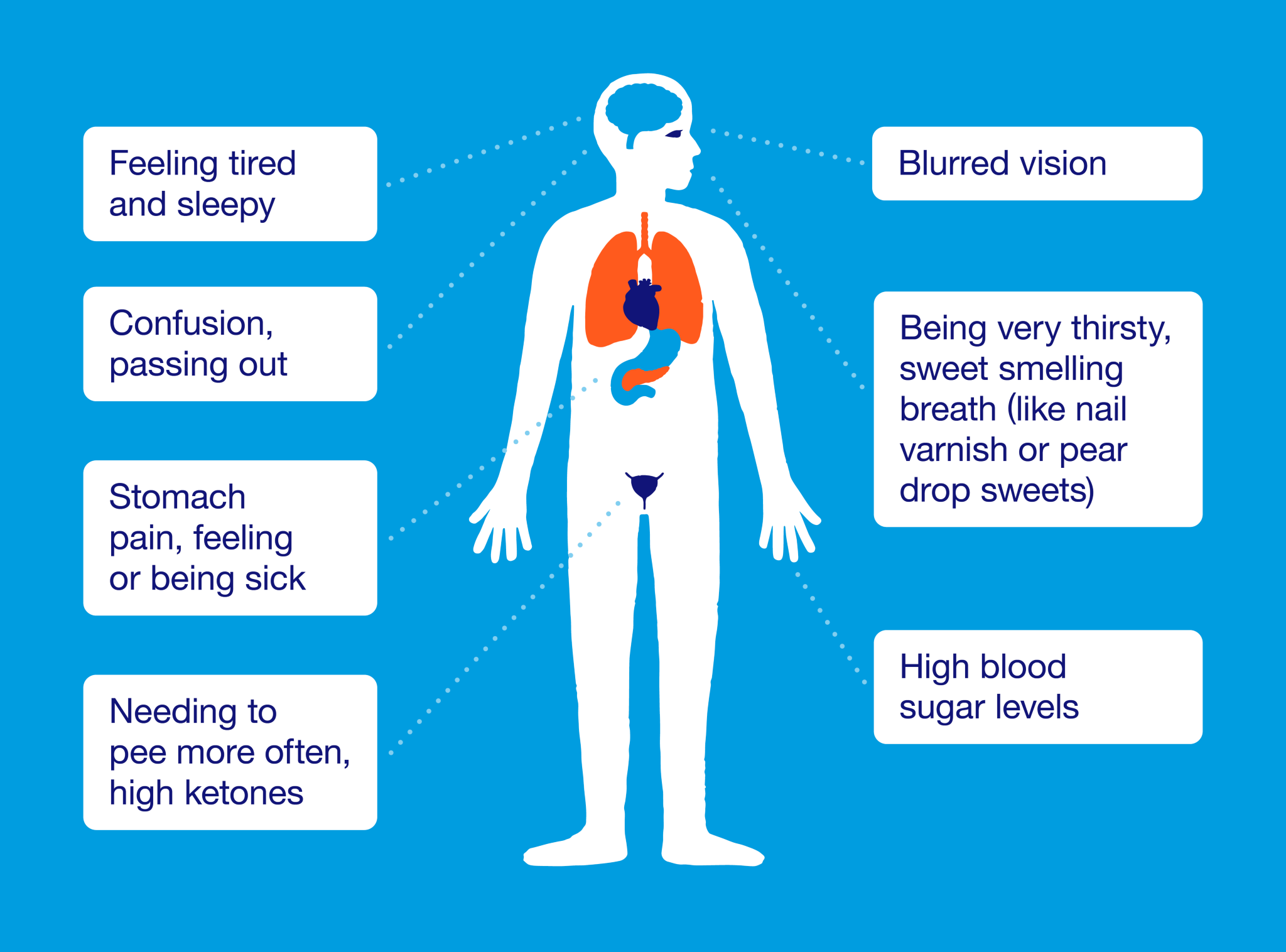
Source © Diabetes UK
Clinical Manifestations
- Hyperglycemia: high blood sugar levels >300 mg/dL (16.7 mmol/L)
- Dehydration
- Ketosis and acidosis
- Acid breath = fruity breath
- Acetone breath
- Polyuria = increased urination
- Polydipsia = increased thirst
- Blurred vision
- Headache
- Fatigue
- Nausea and vomiting
- Abdominal pain
Treatment
Fluid Replacement
This is important for tissue perfusion and assists the kidneys in excreting excess glucose. With rapid IV infusions of 0.9% or 0.45% normal saline, 0.45% normal saline can be used to treat those with hypertension or at risk for heart failure.
After a few hours, when the blood glucose level is 300 mg/dL (16.7 mmol/L), IV 5% dextrose in water is given. It helps prevent a rapid decline in blood glucose levels and allows insulin to do its job.
Correcting an Electrolyte Imbalance
The main electrolyte that is affected is potassium, which must be closely monitored when rehydration therapy begins. Potassium can be given if the serum potassium level drops. Potassium can be withheld if hyperkalemia occurs or the patient is not urinating.
Note: Prescribed potassium is administered intravenously and ensures renal function before administration.
Reversing Acidosis
The breakdown of fat results in the buildup of ketones (acids). The acidosis that occurs in DKA is resolved by the administration of insulin. This will inhibit fat breakdown and stop ketone bodies from building up.
Use short-duration insulin and the prescribed insulin dose, and administer with 0.9% or 0.45% normal saline. Insulin will be administered intravenously until the subcutaneous route begins to avoid a rebound in blood glucose levels.
Note: Monitor potassium and glucose levels and signs of fluid overload. Monitor for signs of increased cranial pressure.
Sources
Diabetic ketoacidosis (DKA): symptoms and treatment | Diabetes UK https://www.diabetes.org.uk/guide-to-diabetes/complications/diabetic_ketoacidosis
Diabetic Ketoacidosis (DKA) Nursing Diagnosis and Care Plan | Nurse Together
Hinkle, J. L., Cheever, K. H., & Overbaugh, K. J. (2022). Brunner & Suddarth’s textbook of medical-surgical nursing (15th ed.), Wolters Kluwer Health
Saunders, N. K. (2023), Saunders NCLEX-RN Comprehensive Review (7th ed.), Elsevier
