A safe nurse must understand what diabetes mellitus is and how it affects the daily living of their patient. This article will give you a thorough understanding of what diabetes is and how best to help your patient.
There are various complications of diabetes mellitus and as a nurse, you’ll need to have an understanding of it and how to prevent complications from arising.
So, without much further ado let’s turn on the heat and begin to learn!
What Is Diabetes Mellitus?
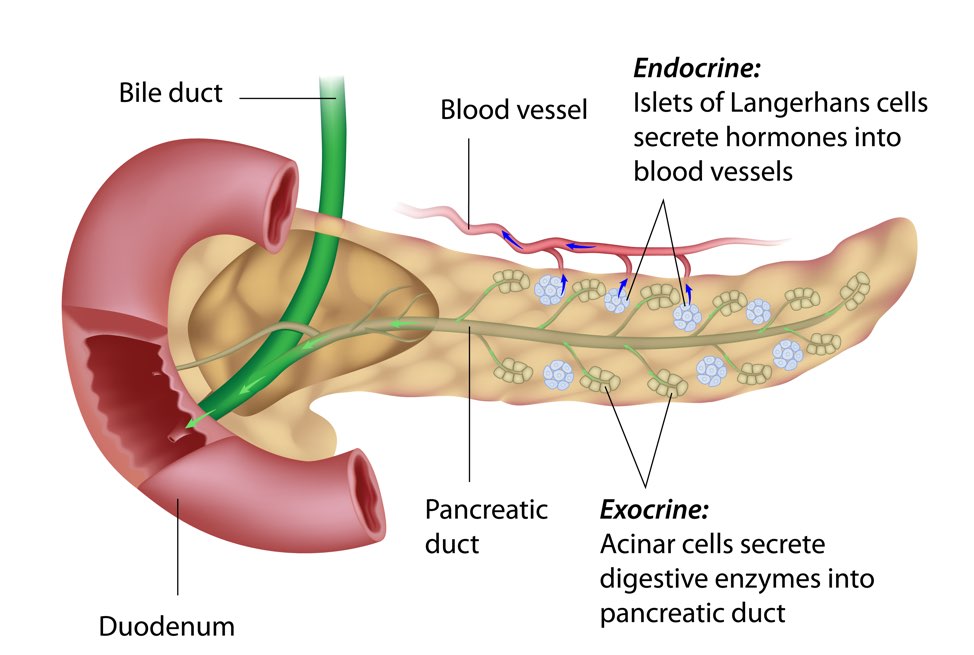
Diabetes mellitus is a metabolic disorder characterized by high blood glucose levels. The pancreas cannot secrete insulin or the cells are unresponsive to insulin receptors. It is associated with other manifestations like hyperglycemia (elevated blood glucose), diabetic ketoacidosis, etc.
Diabetes mellitus is a chronic disorder. There isn’t a cure but it can be managed properly.
Causes of Diabetes Mellitus
- Genetic syndrome
- Liver disease – Liver Cirrhosis
- An autoimmune disease affecting the beta cells in the islets of Langerhans
- A pancreatic disease that destroys the beta islets cells
- Degeneration of Beta cells in islets of Langerhans of the pancreas.
- Hormonal imbalance
Classification Of Diabetes Mellitus
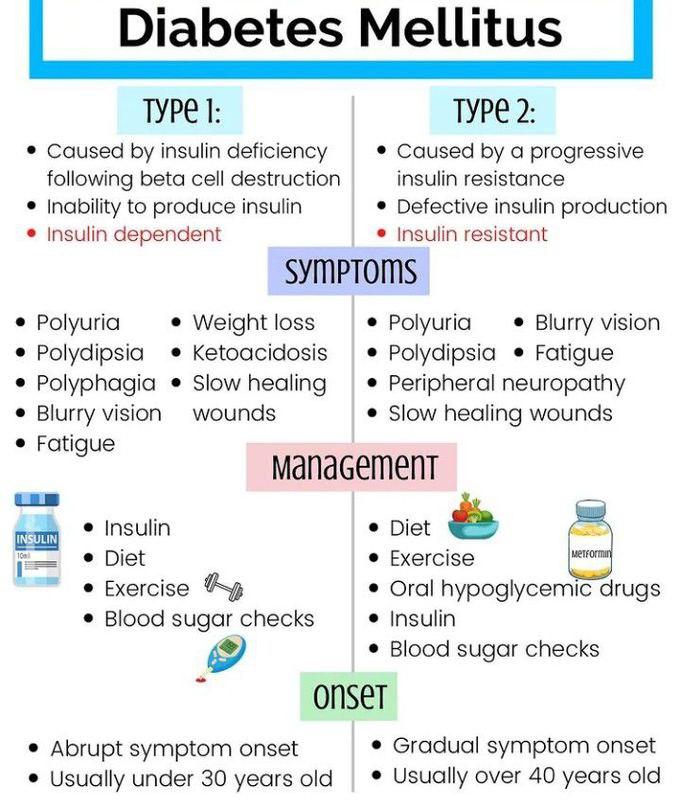
Type 1 Diabetes Mellitus
It is caused by the destruction of the beta cells in islets of Langerhans; it leads to insulin deficiency. It’s also called insulin-dependent diabetes mellitus because people affected require insulin throughout their life.
It is common in people before the age of 40 and it accounts for over 10% of DM cases. It is also called juvenile diabetes because it develops more in infancy or childhood. The beta cells in the islets of Langerhans are not able to produce the insulin needed for glucose absorption.
Type 2 Diabetes Mellitus
It’s common in people over the age of 40. It’s due to insulin resistance (the body cells stop responding to insulin). This causes glucose to float in the blood leading to hyperglycemia.
It accounts for about 90% of diabetic cases and it’s called non-insulin-dependent diabetes mellitus (NIDDM). Only some forms of type 2 DM require insulin while others are managed with oral hypoglycemic drugs, exercise, and diet.
Gestational Diabetes Mellitus
It occurs during pregnancy and the woman experiences hyperglycemia. It’s similar to type 2 diabetes mellitus in terms of insulin resistance.
The reason for the insulin resistance experienced during pregnancy is that placenta hormones counteract insulin which results in glucose Intolerance during pregnancy.
Source © Google
Side Note:
- Diabetes Mellitus is no longer classified as insulin-dependent and non-insulin-dependent because it focuses more on the disease conditions than its etiology.
- Juvenile diabetes doesn’t only occur in childhood or infancy. It can also occur in adults.
Clinical Manifestations
The first symptoms that signify someone is experiencing Diabetes Mellitus are the 3 P’s
- Polyuria – frequent urination
- Polydipsia – increased thirst
- Polyphagia – increased hunger
Other clinical manifestations occur like
- Dehydration
- Tachypnea – increased breath
- Hypovolemia
- Blurred vision
- Weight loss and fatigue
- Nausea and vomiting
- Poor skin turgor
- Dry skin
- Slow wound healing
- Recurrent infections
- Numbness in the hands or feets
Diabetes Mellitus Pathology
Insulin is secreted by the beta cells of the islets of Langerhans in the pancreas. It helps to convert glucose to be stored in the fat, liver, and adipose tissue.
When the insulin level is low or cells no longer respond to insulin or insulin deficiency occurs; glucose remains in the blood. This stimulates negative feedback to the brain to secrete glycogen as glucose. This causes hyperglycemia and can lead to serious complications.
The inability of the kidney to absorb excess glucose leads to glucosuria (glucose in the urine). Polyphagia (increased hunger) occurs because glucose is not stored in the tissues for nourishment and nutrients. Polyuria (excess hunger) occurs due to osmotic diuresis causing dehydration which leads to polydipsia (excess thirst).
The body breaks down fats to give the body energy. This compensatory mechanism leads to ketones causing acidosis which leads to shock, coma, death, etc.
Medication Management
Source © Google
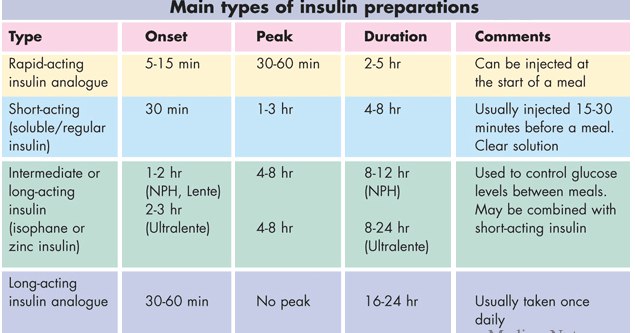
All diabetes mellitus cases have one thing in common – insulin. Though, how it’s managed differs in each case.
Type 1 relies solely on insulin administration. Type 2 involves the use of oral hypoglycemic agents and in some cases such as stress, infection, and surgery will require insulin administration.
There are 4 insulin medications given based on the onset, peak action, and duration. Let’s dive deeper to learn more about them.
- Rapid-acting
It includes insulin lispro (Humalog) and insulin aspart (Novolog). They are called blood glucose-lowering agents. They have an onset of 10 -15 minutes, peak at 1 hour, and last ( duration) 3- 5 hours.
The insulin is clear. Due to the sudden onset, patients are usually advised to eat 5-15 minutes after insulin administration. The short duration of this insulin requires long-acting insulin to maintain blood glucose levels.
- Short-acting
It’s called regular insulin and has an onset of 30 minutes to 1 hour, peak at 2-3 hours, and duration at 4 to 6 hours. It’s a clear solution and is usually administered 20 – 30 minutes before a meal.
It can be given alone or with a combination of long-acting insulin. Examples of short-acting insulin include Humalog R, Novolin R, and Iletin II regular.
- Intermediate-acting insulin
It’s called NPH insulin (Neutral Protamine Hagedorn) or lente insulin. It’s a solution of insulin binding to protamine.
It has an onset of 1 – 2 hours, peaks at 4 – 12 hours, and a duration of 18 – 24 hours. It’s a cloudy solution and examples are Humulin N, Iletin NPH, Humulin L, Iletin L, etc.
- Long- Acting
It’s a crystalline solution with an onset of 1-2 hours, it has no peak hours and it lasts for 24 hours.
It’s a clear solution and cannot be mixed with other insulin. It could lead to precipitation and it’s only given once a day at bedtime. Examples of long-acting are Glargine (Lantus) and insulin degludec (Tresiba).
Side Note: Glargine pH is 4 and mixing it with other insulin alters its pH. It will alter the chemical properties and affect its absorption rate. This is why it is not mixed with other insulin
Pro-tips:
- Insulin is a growth hormone
- Insulin should not be given if blood glucose level is below 90 mg/dl or 5 mmol/L
- Glucose is the antidote for insulin
- Insulin is best absorbed in the abdomen.
- Normal blood glucose level is between 70 -110 mg/dl or 4-8 mmol/L
Complications
- Diabetic nephropathy- damage to the kidney
- Diabetic retinopathy
- Diabetic ketoacidosis
- Neuropathy – damaged nerve
- Heart attack
- Stroke
Sources
Lewis, S. L., Dirksen, S. R., Heitkemper, M. M., Bucher, L., & Camera, I. M. (2020). Lewis’s medical-surgical nursing: Assessment and management of clinical problems (11th ed.). Elsevier.
my.clevelandclinic.org/health/diseases/7104-diabetes
registerednursern.com/diabetes-mellitus-lecture-nclex-review-notes/
rnpedia.com/nursing-notes/medical-surgical-nursing-notes/diabetes-mellitus/